Services
Periodontal Disease
GREAT SMILES ARE BUILT ON HEALTHY GUMS
Services
GREAT SMILES ARE BUILT ON HEALTHY GUMS
The last five years have shown that periodontal health can have a major impact on a patient’s general health. Periodontal disease, a chronic bacterial infection, can lead to a higher incidence of bacteria in the bloodstream, circulating to various organs of the body. These bacteria can then bind with blood platelets and cause an increase in clot formation in arteries and tissues. Those with periodontal disease are at an even higher risk for this to occur.
Periodontal disease occurs when an infection of the gum and/or bone surrounds the tooth. Because the disease is painless, most patients are not aware that they have a problem until examined by a dentist. With a healthy tooth, the root is formed in the jawbone with strong ligaments. This keeps the tooth tightly attached to the bone. The gums protects the bone from bacterial constantly present in the mouth. When healthy, the gum edge is higher than the fiber attachment. In turn, a space is formed around the tooth. This mirrors having a turtleneck sweater.
We all have bacteria in our saliva continuously. When these bacteria collect on all surfaces, plaque forms. If the plaque in the space underneath the gum edge is not removed, infection may occur. The longer that plaque remains on a tooth, the more problems it can cause. Once it hardens, it becomes what’s known as tartar and must be dislodged by a dental professional.
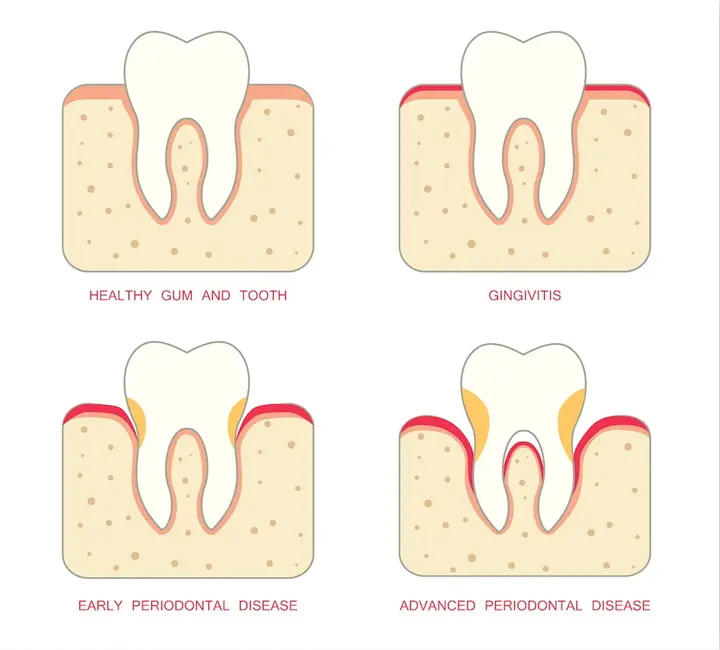
At first, patients experience gum inflammation or gingivitis. As cells are carried to destroy the bacteria, the gum tissue appears red and swollen. Some cases may lead to bleeding when the teeth are being brushed.
The teeth haven’t shown bone destruction, meaning regular brushing and flossing should correct the problem. If not corrected, the bacteria may destroy the fiber barrier and move down the surface of the tooth. Inside lining of the gums and bone are consequently destroyed. A deepened space between the gum and tooth, called a periodontal pocket, is created from the penetration of bacteria. Using a periodontal probe, your dentist can measure the amount of bone loss that has occurred. Bone loss yields a major weakening in tooth support. Eventually, the tooth becomes loose and falls out if the disease goes untreated.
Treating periodontal disease consists of two objectives. The first is to reduce and control bacterial colonies that form beneath the gum edge. Secondly, we want to eliminate any known factors that cause the patient to be more susceptible to further damage. Smoking would be an example.
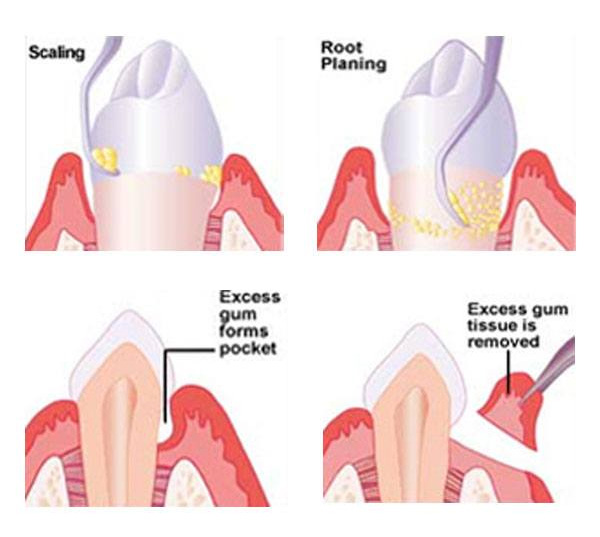
Initially, the pocket depth of the affected gum is typically only slightly deepened. To remove any calculus that has formed, scaling and root planing are done. In order to prevent discomfort, we may numb the gums to protect the tender pockets. Patients must maintain good oral habits following the procedure to keep plaque from reforming. Your oral health will return as soon as the healing gum builds back up around the tooth.
Swollen gums that fail to shrink back to normal must be corrected with a gingivectomy. Patients will experience the same issue if this procedure is not performed.
Actual bone loss takes place in more moderate cases, where the pockets are 5-7 mm in depth. Flap surgery is usually the procedure of choice because of the difficulty in reaching the bottom of the pocket with scaling and root planing. Flap surgery involves an incision made between the gum and tooth. The gum is peeled back away from the neck of the tooth and bone edge. This enables the surgeon to easily see the deep calculus and properly debride the tooth.
An ideal flap surgery results when the periodontist surgically removes the pocket by repositioning the gum down to the new bone level. The surgeon first corrects any irregularities or pitting of the bone and the gum is sutured down to the re-contoured bone. Patients are able to remove the bacterial plaque with brushing and flossing once the pocket is eliminated. As long as patients abide by this daily, the disease is stopped.

A proper diagnosis involves an inventory of the patient’s medical history, clinical examination and x-rays. This allows us to have a better understanding about the disease’s progression rate and enables the surgeon to determine what needs to be done to avoid further breakdown.
Completing a medical history will point us to whether a patient has certain risk factors, resulting in a modified treatment. Below are the most significant general health considerations that may affect susceptibility to periodontal disease.
» Smoking – A host factor that can be altered, smoking greatly increase the risk of disease.
» Diabetes – If not properly controlled, diabetes increases disease risk.
» Stress – Long-term stress may have an adverse effect on how the disease is managed.
» Hormones – Increased estrogen levels connect with an increase in gingival inflammation.
» Medications – Gum overgrowth may be caused by Dilantin and some heart medications.
» Severe Osteopenia – This can lead to more jawbone loss, especially in postmenopausal women.
» Genetics – Nearly 25 percent of the population is susceptible to periodontal disease. We can now conduct a test for genetic susceptibility.

This provides the dentist with a complete picture of the patient’s periodontal condition. We supplement these results with information gained from the x-rays.
The exam helps determine how much bone loss has occurred. A healthy mouth has a 2-3 millimeter space between the tooth and gum. When bacterial plaque causes bone deterioration and penetrates down the side of the tooth, the space deepens into what is called a pocket.
In order to determine the pocket depth, each tooth is measured at six places. This probing does not require anesthesia and gives the dentist a blueprint of periodontal changes.
Patients should also be aware of other important information collected during the examination
» Gum recession – Total bone loss is determined by the amount of recession added to the pocket depth.
» Furcations – Bone loss into the tooth’s furcation compromises the prognosis.
» Amount of attached gingiva – Without properly attached gingiva, recession occurs.
» Occlusion (bite) – Excessive forces on teeth may increase the likelihood of bone loss.
» Tooth mobility (looseness) – This usually indicates inadequate bone support or a bite problem.
» Patient oral hygiene – Long-term results will be compromised by poor brushing and flossing.

Radiographs are mandatory to accurately evaluate periodontal disease. X-rays help determine the amount and location of bone loss, size and shape of the roots, amount of root embedded in the bone, relationship of the teeth to each other, whether a nerve has died, location of sinus and mandibular nerve when placing implants and oral pathologies. Unless gingival grafting is involved, adequate x-rays are a necessity.
Check out the below list of commonly taken x-ray views.
» Full mouth periapicals: 16-18 detailed views of the surrounding bone and teeth
» Panograph: This single screening film shows an overview of the upper and lower jaws, sinus, temporomandibular joint and other anatomic features
» Bitewings: These involve four detailed views of the side and back teeth, specifically used to detect decay. Bitewings are often paired with the panograph by general dentists for routine new patient screenings.
» Vertical bitewings: We conduct four to seven detailed views of the teeth that can show both decay and bone levels when severe bone loss is not prevalent.
» Digital x-rays: Stored on a computer, these are generally available in periapical and bitewings only.
Patients can rest assured that film speed has improved dramatically; meaning that very little radiation is needed to expose the x-ray film. Experts estimate that the amount of body radiation received with a full mouth series is less than one would receive from a day at the beach.

Once this stage is reached, your periodontist will organize and systematically evaluate the results to make a diagnosis. Patients must realize that while there may be approaches to treat a problem, only one correct diagnosis exists. Various treatment options will formulate once a diagnosis is determined.

In order to yield a successful result, both the calculus and plaque must be removed. We will also create an environment that ensures an easy plaque removal process. We may also address the following at this point.
» Demonstration of proper oral hygiene habits to remove surface plaque
» Scaling and root planing to remove calculus and plaque
» Removal of hopeless teeth to ensure optimal results
» Adjustment of bite if necessary
» Gingivectomy – When the bone contour has not been altered, trimming excess tissue is needed.
» Flap surgery – This gives the periodontist access to the jawbone. The most advanced cases require smoothing irregularities that were caused by infection.
» Regeneration surgery – Since the regeneration of tissue and bone are not always possible with periodontal therapy, new techniques are allowing for more predictable tissue regeneration.
Ultimately, the surgeon wants to reduce pocket depth. Pocket elimination, where patients can remove plaque from the sulcus daily, is the ideal goal. However, deeper pockets may still have some depth postoperatively. As long as these teeth don’t jeopardize the surrounding dentition, they can usually be maintained during the procedure.
Patient home care and regular periodontal maintenance are the two most important factors in determining long-term success. Without routine maintenance, there is a 20-fold increase in the likelihood of recurrent disease. Our doctors recommend cleanings every three months instead of biannual appointments. These are usually alternated between the general dentist and periodontist. Consistent flossing and brushing are critical to ensuring your overall periodontal health!
PERIODONTAL
MAINTENANCE
AND FOLLOW UP CARE
Good periodontal health is maintained with good oral hygiene and regular cleanings. Research proves that those who fail to maintain quality dental habits have 20 times the amount of bone loss as those who do. To prevent reoccurrence of periodontal disease, it is vital that patients remove plaque twice daily. Maintaining good dental habits and regular cleanings are critical to long-term oral health. Without adequate follow-up care, the disease will come back. That’s why the patient must take full responsibility for their periodontal health.
In cases where some residual pockets are deeper than 3 mm, or where the patient has exhibited a high susceptibility to breakdown, it is critical that we perform three-month recalls. This is done to manage the bacteria from forming plaque immediately after treatment. Read more
Plaque usually takes about three months to develop into an aggressive infection. While minimal bone loss takes place within the first three months, the likelihood of breakdown dramatically increases after 90 days. The aggressiveness of plaque will be kept to a minimum as long as plaque is regularly removed.
The two mainstays of oral hygiene are brushing and flossing. Patients should slide the bristles of the brush into the cuff of the gum, like a broom may slide under the edge of the refrigerator. Positioned at a 45 degree angle to the tooth, move the brush in a circular motion. This method is the best way to remove plaque from beneath the gum edge. We do not recommend a scrubbing motion, as this may lead to gum recession.
Update of dental and medical history
Soft tissue cancer exam
Clinical decay examination
Clinical periodontal examination
Review of proper oral hygiene as needed
Scaling above gum level
Root planing under gum level
Polishing
Every three months, we take full mouth radiographs to determine the stability of the bone level.
A key observation at the appointment will be whether the tissues bleed when probed. No bleeding leads to a healthy mouth. Additional treatment will be warranted if bleeding does exist. We will also take note if the x-rays show a change of bone level.
Throughout the periodontal maintenance appointment, we want to make sure that patients are comfortable. We have nitrous oxide available for those who need help relaxing